Liver Transplantation
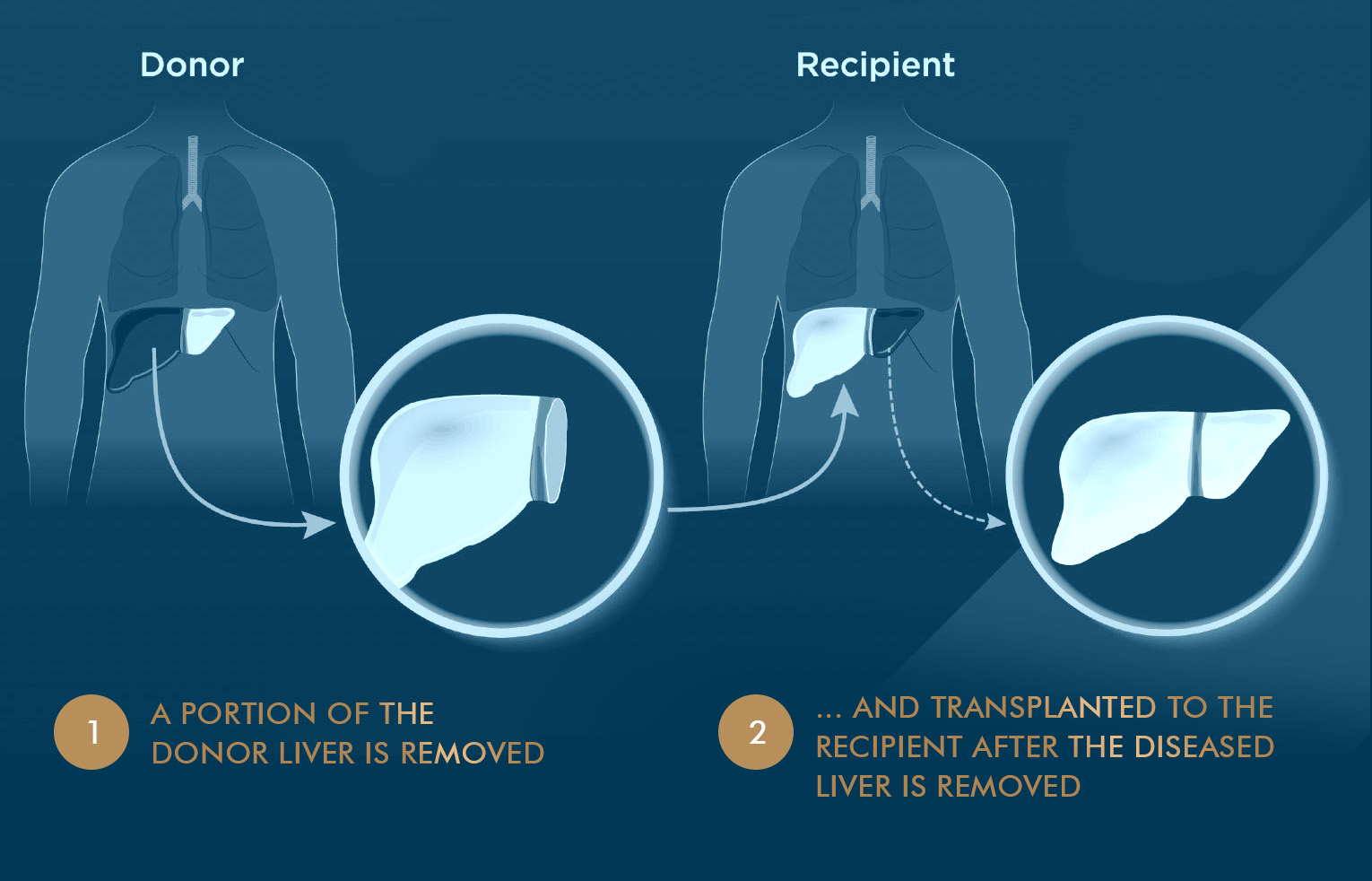
A liver transplant replaces a diseased liver with a healthy liver. The new liver may be from a donor who has recently died (deceased donor) or a healthy living donor. There are two main types of liver transplant:
Before undergoing liver transplantation in Singapore, patients must complete a series of pre-transplant assessments to ensure their suitability for the procedure. This includes consultations, diagnostic imaging tests and blood work. Results of these pre-assessments will help doctors check how severe the illness is, how urgent the need for a transplant is.
In Living Donor liver transplant, the most appropriate donor will be selected, counselled and undergo a series of pre-transplant assessments to ensure their suitability for the procedure. The blood type and body size of the donor have to match the person receiving the transplant.
During transplant surgery, the transplant team replaces the diseased liver with a donated, healthy liver. Liver transplant surgery usually takes between 6 - 12 hours.
After the transplant surgery, the recipient may need to stay in the hospital for several weeks while the transplant team monitors how well the body is accepting the new liver. Medicines will be given to control any pain and prevent infection. The recipient will start taking immunosuppressive medicine to prevent rejection of the new liver.
Donor usually stays about a week or less in laparoscopic cases.
It is important for the recipient and caregivers to be familiar with the medicines and to report any side effects. After a liver transplant, the recipient will undergo regular blood tests and occasional liver biopsies to make sure there is no rejection of the new liver. It is very important to have regular follow-up with transplant team.
In Singapore, for Deceased donor liver transplant, the donor is Singapore citizen or
Permanent residents (PR) who has recently passed away (brain death). All Singapore
Citizens & PR who meet the age requirement and are of sound mind will be
automatically included as a potential organ donor unless they have opted out.
If deem suitable, the hospital will identify the brain-dead patient as a potential
donor. This is the most commonly performed transplant procedure in which the liver
is procured from a patient after brain death is certified. The recipient will be the
most suitable patient on the top of the National waiting list, prioritized by the
medical urgency and waiting time. This program is only applicable for Singapore
citizens or Permanent residents (PR) and only performed in the public hospitals.
In Living donor liver transplant, a relative, someone who has a close emotional bond
or an altruistic person can be considered as potential donors. The most appropriate
donor will be selected, counselled and undergo a series of pre-transplant
assessments to ensure their suitability. This can be performed for all patients
including foreign patients. Living donor transplant provide an alternative for
patients as there is a shortage of deceased donors.
Mount Elizabeth Hospital is the only accredited private Liver transplant centre in
Singapore.
A liver transplant, like all major surgery, has possible serious risks such as bleeding, infection, and complications from anaesthesia. In addition, people who have a liver transplant may have side effects from the immunosuppressive drugs they need to take. These medicines weaken the immune system so the body does not reject the new liver. This also means that a patient may be at increased risk of developing infections. Some of the immunosuppressive drugs can also cause high blood pressure and cholesterol, diabetes, and weaken the bones and kidneys. Regular health checks with the transplant team are important after a liver transplant.
Liver transplantation is generally very successful. Most people are able to return to their daily routine
within a few months after the transplant, and many of them earlier. Transplant success depends on a number
of variables, including health status, age and nature of disease. The overall survival of patients at 1 and
5 years is above 90% and 70% respectively. Without the transplant, many patients will not survive for more
than 6 - 12 months due to disease progression.
A common cause of organ failure following a transplant is due to patients not following the prescribed
immunosuppression medication regimen. Careful attention to medication schedules, lifestyle changes, diet
and close follow-up with the transplant team and primary care physician is important.
Living donation significantly decreases the time a patient has to wait for a liver on the National waiting
list, prior to the worsening of the patient’s condition. Livers from living donors are usually of excellent
quality because donors are carefully evaluated prior to donation and are only allowed to donate if they are
in good health.
The criteria for Living Donor Liver transplant are more liberal than the criteria for the deceased donor
program in many centres, extending the eligible pool of patients who can potentially benefit.
The deceased liver transplant program in Singapore is a national program and is only available in public
hospitals and requires both recipient and donor to be Singapore citizens or PR. The average waiting time
for an available deceased organ in Singapore is about 12 months vs. 2 months for a living donor liver
transplant once a donor is deemed suitable.
As with any major surgery, a liver donation carries risks. These include temporary jaundice, bleeding,
infection, bile leakage and even death (very rare). However, most donors do very well and those with no
complications can usually be discharged within a week and make a full recovery in a few months. Donors are
well looked after by the transplant team inpatient and through outpatient follow-ups.
All potential living donors will be informed and well counselled about the donation process, possible
outcomes, risks and post-donation care.
The transplant team is not allowed to find a donor on behalf of the patient. Organ trading is prohibited in Singapore and internationally. Anyone who is involved in the buying or selling of organs can be prosecuted by law.
Yes, a person can choose who the intended recipient is, as long as the assessments have deemed that the
person is healthy and a match to the recipient, and a completely voluntary decision is made without
coercion or financial promises. A non-related person may also choose to be an altruistic donor. Individuals
may also donate to any patient on the national waiting list i.e., they do not specify the recipient
(non-directed donors).
Once the evaluation is complete and cleared, the application will be reviewed by the Transplant Ethics
Committee (TEC) under the auspices of the Ministry of Health, Singapore (MOH) to ensure it is appropriate.
There is a compulsory cooling-off period after the review. The transplant surgery can go ahead after the
TEC’s approval.
A donor can withdraw from organ donation any time, for any reasons and the decision will be kept
confidential.
In Singapore, the Human Organ Transplant Act (HOTA) allows for payments to living donors, only for reimbursing or defraying the expenses or loss of earnings that may be reasonably incurred as a result of organ donation. This includes costs for health checks, tests, surgery, follow-up visits and indirect costs such as loss of earnings.
Dr. Lee is a double USA-fellowship trained Hepatopancreatobiliary and liver transplant surgeon. He is a Ministry of Health, Singapore (MOH) gazetted and Board-accredited Liver Transplant surgeon. He trained as a Hepatopancreatobiliary and Liver Transplant fellow for more than a year in New York-Presbyterian Hospital, which is an international leader in the organ transplantation with the most transplant surgeries performed in the United States.
Our multidisciplinary liver transplant team in Mount Elizabeth is the only private liver transplant centre in Singapore.
Our focus is on optimizing your overall health while waiting for a liver, minimizing your time on the waitlist, and achieving optimal long-term health outcomes with a good quality of life. Our team includes a dedicated transplant coordinator, transplant surgeons, hepatologists (physicians who specialise in liver disease), critical care specialists, psychiatrists as well as a strong nursing and allied health team (pharmacists, nutritionists, physiotherapist, social workers).
Liver transplantation requires life-long care. Our compassionate team provides personalized care every step of the journey—from the uncertainty of waiting for a liver, to the hospital stay and your long-term follow-up care. We partner closely with you and your family with the goals of helping you spend less time in the hospital and more time living life.
Find out more here.

MBBS, MMed (Surgery), MSc, FAMS, FRCSEd
Prior to private practice, liver surgeon Dr Lee Ser Yee was a founding member and Senior Consultant at the Department of Hepatopancreatobiliary (HPB) and Transplant Surgery at Singapore General Hospital (SGH). He served as the Director of the Laparoscopic programme and the Director of the Surgical Skills Training Program and the SingHealth Surgical Skills Centre.
He started his medical training at the National University of Singapore in 1996 and completed his training in General Surgery, HPB surgery and Liver Transplantation at SGH and National Cancer Centre, Singapore.
He also completed dual USA-fellowships in Advanced Laparoscopic HPB surgery and Liver Transplantation under Professor Daniel Cherqui at the New York Presbyterian Hospital-Weill Cornell Medical Center and a Complex Surgical Oncology clinical fellowship at Memorial Sloan Kettering Cancer Center in New York.


Mount Elizabeth Medical Centre
#08-07, 3 Mount Elizabeth, Singapore 228510
Tel: 6454 0054
|
Fax: 6764 0054
|
Email: ask@surgicalassociates.sg
Gleneagles Medical Centre
#05-01, 6 Napier Road, Singapore 258499
Tel: 6471 0054
|
Fax: 6271 0054
Need medical advice from Dr Lee or Dr Tan? Leave us a message and we will attend to you within one working day.