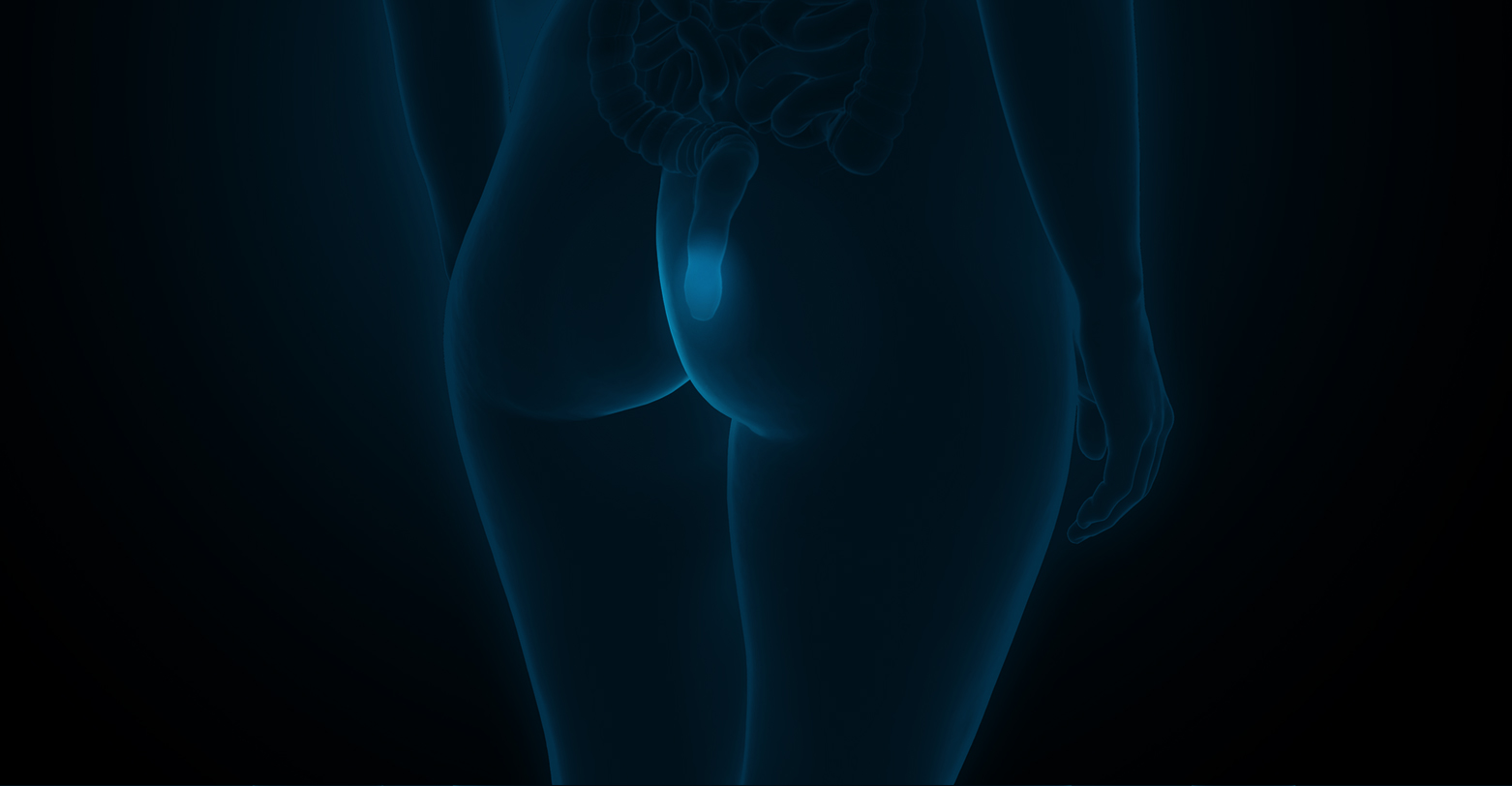
Types of IBD include
- Ulcerative colitis
This condition causes inflammation and ulcers that involves the innermost lining (mucosa) of the colon and rectum. The rectum is always affected, with variable involvement of the colon depending on the severity of the disease. - Crohn’s Disease
This condition can involve any part of the gastrointestinal tract, including the mouth, esophagus, stomach, small intestine, colon, rectum and even the anus. The inflammation can involve all the layers of the wall of the affected organ, with the small intestine and colon being the most commonly affected regions.
What are the symptoms of IBD?
The symptoms of IBD vary, depending on where it occurs and the severity of the inflammation. Some symptoms common to both ulcerative colitis and Crohn’s disease include:
- Bloody diarrhoea
- Abdominal pain
- Weight loss
- Fatigue
- Anaemia
There may also be associated inflammation of the joints (arthritis), eyes (iritis), bile ducts (primary sclerosing cholangitis), lung (pleuritis) and skin.
What causes IBD?
The exact cause of IBD remains unknown, with an interplay of genetic and environmental factors playing a part in its development. These factors include:
- Genetics
There is a higher risk of developing IBD if there is a family history of these conditions but the majority of patients do not have a family history. - Affluence
IBD increases with industrialization of a country, indicating that environmental factors such as a diet high in fat or refined foods may play a role. - Race/ethinicity
IBD can occur in any race, although whites, and particularly Ashkenazi jews are at a higher risk. Over the last few decades, however, there has been an increasing incidence of IBD in Asia, possibly related to westernization of lifestyle, industrialization, changes in diet, etc. - Smoking
Smoking increases the risk and severity of Crohn’s disease. - Use of antibiotics in childhood
There is some evidence that antibiotic use early in life may increase the risk of IBD. - Non-steroidal anti-inflammatory drugs (NSAIDs)
These medications may increase the risk of developing IBD or worsen disease in patients who have IBD.
Interestingly, there is some evidence that prior appendectomy seems to be protective for ulcerative colitis.
What are the complications associated with IBD?
- Cancer
IBD increases the risk of cancer, particularly colorectal cancer and to a lesser extent, small intestinal cancer. As such, regular colonoscopies are required for surveillance. - Bowel perforation
- Intra-abdominal infections with abscess and fistula formation
- Narrowing (stricture) and obstruction of the bowel
- Perianal fistula formation in Crohn’s disease
- Higher risk of developing blood clots in veins and arteries
- Toxic megacolon, a life-threatening dilation of the colon secondary to severe inflammation
How is Inflammatory Bowel Disease (IBD) Diagnosed?
The following tests may be performed to rule out other causes for your symptoms before confirming the diagnosis of IBD.
- Blood tests
-
Stool tests
-
Fecal calprotectin
This is a marker of bowel inflammation and can be used to support the diagnosis of IBD, as well as to diagnose flares of the disease. - Stool cultures and stool tests for parasites to rule out infective causes of your symptoms
-
Fecal calprotectin
-
Endoscopic procedures
-
Colonoscopy
This allows examination of the colon, rectum and terminal ileum. -
Gastroscopy
This allows examination of the esophagus, stomach and the duodenum (first part of the small intestine). While it is not common for these areas to be affected by Crohn’s disease, this may be recommended if you have symptoms such as nausea, vomiting, upper abdominal pain or poor appetite. -
Double balloon enteroscopy
This may be required if the diagnosis has not been established despite gastroscopy and colonoscopy. It allows examination of the small bowel where standard endoscopies do not reach.
Biopsies of the inflammed bowel taken during these endoscopic procedures can help to confirm the diagnosis of IBD. -
Colonoscopy
-
Radiologic procedures
-
Computed Tomography (CT)
CT enterography is used to evaluate the small bowel, while CT abdomen/pelvis may be performed if there is suspicion of an abscess or perforation of bowel. -
Magnetic Resonance Imaging (MRI)
This is used to evaluate the small bowel (MR enterography) as well as perianal fistulas (MRI pelvis).
-
Computed Tomography (CT)
What Are the Treatments for Inflammatory Bowel Disease (IBD)?
-
Medications
The mainstay of treatment of IBD is with medications. The aim of treatment is to reduce inflammation, achieve long term remission and reduce the development of complications. These medications frequently have to be taken lifelong.
Some classes of medications that may be used include
- Aminosalicylates
- Corticosteroids
- Antibiotics
- Immunosupressants
- Biologics
-
Surgery
Approximately 20% of patients with ulcerative colitis have severe symptoms that may eventually require surgery. The surgery involves removal of the entire colon and rectum (panproctocolectomy) and the formation of an ileo-anal pouch to restore intestinal continuity and bowel function. Although the surgery is a major one, the disease is cured after surgery and no IBD medications are required subsequently.
On the other hand, up to 90% of patients with Crohn’s disease may require at least one surgery in their lifetime. The type of surgery required depends on the part of the gastrointestinal tract affected by Crohn’s disease. Surgery for Crohns disease is performed to address complications of the disease, as surgery is not curative and life-long medications are still required even after surgery.
Surgeries for patients with IBD should be performed laparoscopically if possible, with many studies showing better outcomes such as reduced complication rate, shorter hospital stay, better cosmesis and reduced risk of adhesion formation and hernia development, as compared with open surgery.

